Skip to contentpatient, credentialing, prior authorization, electronic health record, medical billing, what is denial in medical billing, revenue, medical necessity, reimbursement, policy, audit, physician, diagnosis code, health care provider, contract, automation, health insurance, revenue cycle management, knowledge, cash, organization, medical record, cash flow, robotic process automation, appeal, workflow, analytics, healthcare industry, current procedural terminology, communication, medicaid, root cause analysis, health care, denial, document, outsourcing, remittance advice, diagnosis, remittance, owner, medical billing services, medical billing audit, outsourced medical billing, insurance coverage, medical billing company, insurance company, medical billing medical, medical coding, medical billing software, fee, adjudication, failure, patient satisfaction, reason, electronic remittance advice, understanding, therapy, patient portal, deductible, clinical laboratory improvement amendments, expert, social security number, explanation of benefits, attention, primary care, data entry, copayment, utilization management, percentage, risk, denial in medical billing, billing and coding, claims denial, billing services, insurance payer, dental insurance verification, insurance verification, healthcare common procedure coding system, accounting, evaluation, strategy, denials in medical billing, health information management, managed care, productivity, data analysis, evidence, medical device, database
Frequently Asked Questions
How to handle co47 denial in medical billing?
Handling a CO47 denial in medical billing involves identifying the reason for the denial, usually related to timely filing issues or incomplete documentation. Ensure you review the claims thoroughly and resubmit with corrected information or appeal the denial if justified.
How does denial work in medical billing?
Denial in medical billing occurs when a healthcare claim is rejected by an insurance provider due to issues such as incomplete information, coding errors, or lack of authorization, which prevents the provider from receiving payment for services rendered.
How to calculate denial rate in medical billing?
To calculate the denial rate in medical billing, divide the number of denied claims by the total number of claims submitted, then multiply the result by 100 to express it as a percentage. This metric helps assess the efficiency of your billing processes.
How to handle duplicate denial in medical billing?
Handling duplicate denial in medical billing involves promptly reviewing claims to identify the reason for the denial, correcting any errors, and resubmitting the claims with proper documentation. Ensure to track all communications and maintain thorough records.
How to resolve cob7 denial in medical billing?
Resolving a COB7 denial in medical billing involves reviewing the claim for accuracy, ensuring correct coordination of benefits, and providing any missing information regarding insurance coverage. Resubmit the claim with the necessary documentation to facilitate payment.
How to deal with va denial to pay medical bill?
Dealing with a VA denial to pay a medical bill involves reviewing the denial details, gathering necessary documents, and filing an appeal if justified. Ensure that all patient information and coding are accurate to strengthen your case.
How to reduce denials in medical billing?
Reducing denials in medical billing involves implementing accurate patient information collection, ensuring proper coding, and verifying prior authorization. Regular staff training and utilizing denial management software can also significantly enhance claim success rates.
How to handle denials in medical billing?
Handling denials in medical billing involves identifying the denial reason, gathering necessary documentation, correcting errors, and resubmitting the claim promptly. Establishing a denial management process can prevent future issues and improve revenue recovery.
How many types of denials are there in medical billing?
There are primarily two types of denials in medical billing: soft denials and hard denials. Soft denials are temporary issues that can often be resolved, while hard denials indicate more permanent reasons for rejection, requiring more extensive appeals or changes.
What causes co47 denial in medical billing?
The causes of CO47 denial in medical billing are primarily related to billing issues, such as submitted charges not being covered under the patient’s plan or services that are deemed not medically necessary by the insurer.
How can I prevent denial occurrences?
Preventing denial occurrences involves ensuring accurate patient information, thorough coding practices, and obtaining prior authorizations when needed. Regular staff training and clear communication with payers also play a crucial role in minimizing claim denials.
What strategies assist in denial resolution?
Strategies that assist in denial resolution include thorough documentation, timely appeals submission, and effective communication with payers. Implementing these tactics helps healthcare providers address denials swiftly and improve overall claim acceptance rates.
How to track denied claims efficiently?
Tracking denied claims efficiently involves implementing a systematic approach to monitor and analyze denials. Use specialized software to automate tracking, categorize denials by reason, and regularly review metrics to identify patterns for proactive resolution.
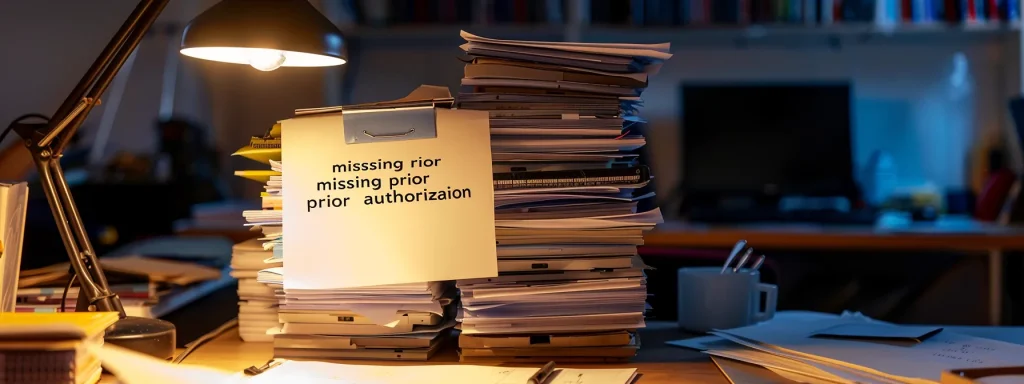
What documents are needed for denial disputes?
The documents needed for denial disputes include the original claim, any correspondence from the insurance company regarding the denial, and supporting documents such as medical records and patient billing information relevant to the claim.
How do coding errors lead to denials?
Coding errors lead to claim denials by causing discrepancies between the submitted billing codes and the patient's services provided. These inaccuracies can lead insurers to reject claims due to invalid coding, resulting in delayed payments and revenue loss for healthcare providers.
What are common denial codes to know?
Common denial codes to know include CO-16 (Claim Lacks Information), CO-27 (Expenses Incurred After Coverage Terminated), and CO-50 (Billing Requirement Not Met). Understanding these codes can help healthcare providers address issues and reduce claim denials effectively.
How do adjustments affect denial management?
Adjustments significantly impact denial management by enabling healthcare providers to correct billing errors and reduce the likelihood of claim denials. By properly implementing adjustments, practices can enhance accuracy in claims processing and ultimately improve their revenue recovery efforts.
What is the impact of late denials?
The impact of late denials is significant; they lead to delayed revenue recovery, increased administrative costs, and can adversely affect cash flow for healthcare providers. Timely resolution of denials is crucial for maintaining financial stability.
How to train staff on denial handling?
Training staff on denial handling involves equipping them with knowledge about common denial reasons, proper coding practices, and effective communication techniques. Regular workshops and practical exercises can enhance their skills in resolving claims efficiently.
What technology aids in denial prevention?
Technology that aids in denial prevention includes advanced billing software, coding automation tools, and integrated eligibility verification systems. These solutions help ensure accurate claims, streamline data collection, and facilitate proper authorization, ultimately reducing the risk of claim denials.
How to conduct denial trend analysis?
Conducting denial trend analysis involves systematically collecting and reviewing denied claims data. Analyze this data to identify patterns or common reasons for denials, enabling you to implement targeted strategies to reduce future claim rejections.
What role does patient information play in denials?
Patient information plays a crucial role in claim denials. Incomplete or inaccurate patient data can lead to rejected claims, as insurers require precise details for processing. Ensuring accurate patient information is essential for minimizing denials and optimizing revenue recovery.
How long does it take to resolve denials?
The timeframe for resolving denials varies based on the reason for the denial and the efficiency of the appeals process, but typically it takes anywhere from a few days to several weeks to achieve resolution.
What are best practices for denial follow-ups?
The best practices for denial follow-ups include identifying the root cause of denials, reaching out promptly to payers, maintaining thorough documentation, and establishing a systematic process for tracking and resolving issues to enhance revenue recovery.
How can effective communication reduce denials?
Effective communication can significantly reduce denials by ensuring that all necessary patient information is accurately conveyed and clarifying any ambiguities with payers. This proactive approach minimizes errors and enhances clarity, leading to a smoother claims process.
What resources aid in understanding denial types?
Resources that aid in understanding denial types include comprehensive billing guides, professional training programs, and industry webinars. Additionally, collaborating with experienced medical billing specialists can provide valuable insights into specific denial scenarios and effective resolution strategies.
How do regulations influence denial processes?
Regulations significantly influence denial processes by establishing criteria for claim approvals, defining valid coding practices, and setting guidelines for necessary documentation. Compliance with these regulations is essential for minimizing denials and optimizing claims processing in medical billing.
What role do appeals play in denials?
The role of appeals in denials is crucial; they provide a formal process to challenge and rectify denied claims, increasing the chances of recovering lost revenue for healthcare providers through correct documentation and supporting evidence.
How to ensure compliance in billing practices?
Ensuring compliance in billing practices involves staying updated on healthcare regulations, regularly training staff on coding and billing procedures, and conducting thorough audits to identify and correct any discrepancies proactively.
What metrics evaluate denial management effectiveness?
The metrics that evaluate denial management effectiveness include the denial rate, reasons for denials, appeal success rate, and the time taken to resolve claims. Analyzing these metrics helps healthcare providers improve their billing processes and revenue recovery.
denial in medical billing, medical billing services, revenue cycle management, Insurance verification, Medical billing and coding for mental health, Medical billing outsourcing, Insurance Pre-Authorization, Denial management, medical billing services in nj, remote medical billing, medical billing jobs, Eligibility Verification, Medical billing near me, HIPAA-compliant billing, medical coding solutions, healthcare billing solutions, reasons of denials, medical billing specialist, authorization denial in medical billing, denial reasons in medical billing, denials in medical billing, medical billing denials, what is denial in medical billing, Medical billing software for small business, Best medical billing software for small business, Affordable medical billing software for small business, Medical billing software for startups, Cloud-based medical billing software for small business, Easy-to-use medical billing software, Medical billing software pricing for small business, Top medical billing software for small practices, Medical billing and coding software for small business, Small business healthcare billing solutions, HIPAA-compliant medical billing software, Online medical billing software for small business, Medical billing software comparison for small business, Free medical billing software for small business, Medical billing software features for small business, Medical billing software for solo practitioners, Electronic medical billing software for small clinics, Best cloud medical billing software for small business, Small business-friendly medical billing software, Medical billing automation software for small business., common denials in medical billing, cardiology medical billing services Pittsburgh, hematology billing services, general surgery medical billing services, ENT medical billing services, orthopedic medical billing services, gastroenterology medical billing services, urology medical billing services, medical billing services Delaware, medical billing companies in Los Angeles, medical billing services in Dallas TX, radiology medical billing services, dermatology billing services, emergency room billing services, dental billing services, mental health billing services, nephrology billing services, ophthalmology billing services, pathology billing services, pediatric medical billing services, podiatry billing services, pulmonology billing services, rheumatology billing services, chiropractic billing services, physical therapy billing services, occupational therapy billing services, speech therapy billing services, anesthesia billing services, pain management billing services, oncology billing services, endocrinology billing services, infectious disease billing services, internal medicine billing services, neurology billing services, obstetrics and gynecology billing services, allergy and immunology billing services, plastic surgery billing services, psychiatry billing services, sports medicine billing services, urgent care billing services, vascular surgery billing services, wound care billing services, medical billing services New York, medical billing services Chicago, medical billing services Houston, medical billing services Phoenix, medical billing services Philadelphia, medical billing services San Antonio, medical billing services San Diego, medical billing services Dallas, medical billing services San Jose, medical billing services Austin, medical billing services Jacksonville, medical billing services Fort Worth, medical billing services Columbus, medical billing services Charlotte, medical billing services San Francisco, medical billing services Indianapolis, medical billing services Seattle, medical billing services Denver, medical billing services Washington DC, medical billing services Boston, medical billing services El Paso, medical billing services Nashville, medical billing services Detroit, medical billing services Oklahoma City, medical billing services Portland, medical billing services Las Vegas, medical billing services Memphis, medical billing services Louisville, medical billing services Baltimore, medical billing services Milwaukee, medical billing services Albuquerque, medical billing services Tucson, medical billing services Fresno, medical billing services Sacramento, medical billing services Kansas City, medical billing services Atlanta, medical billing services Miami, medical billing services Omaha, medical billing services Raleigh, medical billing services Colorado Springs, medical billing services Virginia Beach, medical billing services Long Beach, medical billing services Oakland, medical billing services Minneapolis, medical billing services Tulsa, medical billing services Tampa, medical billing services Arlington, how many denials in medical billing, hard denials in medical billing
patient, outsourcing, medical billing, revenue cycle management, physician, health insurance, electronic health record, accounts receivable, revenue, reimbursement, audit, cardiology, surgery, credential, medical record, internal medicine, healthcare industry, health insurance portability and accountability act, radiology, fee, cash, cash flow, general surgery, customer, urology, health care, new york city, contract, outsourced medical billing, billing services, medical billing services, medical billers, outsourcing billing services, service medical billing, medical billing companies, medical billing experts, medical billing specialists, medical billing solutions, medical coding online, medical coding from home, billing and coding online, kareo billing, chiropractic billing services, medical coding and billing certificate, medical coding companies, medical coding and billing online program, private practice billing services, medical coding and billing, billing company, billing specialist, dme billing, medical coding services, podiatry billing services, anesthesia billing, healthcare billing, nursing, knowledge, family medicine, efficiency, pain management, gastroenterology, customer service, medicare, plastic surgery, analytics, pain, emergency medicine, anesthesiology, therapy, workflow, primary care, optometry, web browser, immunology, patient satisfaction, ambulance, productivity, turnover, performance indicator, medicaid, primary care physician, understanding, overhead, pulmonology, onboarding, regulation, emergency, new jersey, pathology, medical claims specialist, medical claims, urgent care billing, risk, prior authorization, managed services, organization, automation, regulatory compliance, debt, robotic process automation, rcm system, healthcare revenue cycle, rcm, machine learning, ambulatory care, current procedural terminology, intelligence, bad debt, preregistration, accounting, research, workforce, patient safety, policy, leadership, innovation, predictive analytics, medical billing and coding, certification, american health information management association, exam, professional certification, associate degree, employment, health information technology, health information management, healthcare common procedure coding system, humanities, disease, anatomy, medical terminology, diploma, computer program, international classification of diseases, skill, physiology, ethics, training, profession, coding certification, medical biller, certified billing, medical coding certifications, coding certificate program, online billing and coding, certified medical coder, ahima medical coding, billing coding, billing and coding, certified professional coder, certified billing and coding specialist, medical coding specialist, becoming a medical coder, coding specialist, billing and coding specialist, professional coder, nursing home, information technology, national healthcareer association, curriculum, statistics, bureau of labor statistics, pharmacology, accreditation, credit, mathematics, salary, social science, aapc medical coding, cpt codes, medical coding, certified coding specialist
Frequently Asked Questions
How do revenue cycle management companies make money?
Revenue cycle management companies generate income by charging healthcare providers a percentage of the claims they process or a fixed fee for their services. They also benefit from improving cash flow and reducing the time taken to collect reimbursements.
How do healthcare facilities optimize functionality with revenue cycle management?
Healthcare facilities optimize functionality with revenue cycle management by streamlining billing processes, enhancing patient data accuracy, reducing claim denials, and improving financial reporting, ultimately leading to increased revenue and operational efficiency.
How can a healthcare organization improve its revenue cycle management?
Improving revenue cycle management for a healthcare organization involves optimizing billing processes, enhancing claim submissions, implementing effective denial management strategies, and leveraging technology for accurate coding and billing practices. Regular training and data analysis also contribute to maintaining efficiency.
Do bundled payments simplify revenue cycle management?
Bundled payments can simplify revenue cycle management by consolidating multiple services into a single payment, reducing administrative complexity and streamlining billing processes. This approach enhances efficiency and potentially improves cash flow for healthcare providers.
How does health information technology and management relate to the revenue cycle?
Health information technology and management are integral to the revenue cycle as they streamline processes, enhance data accuracy, and facilitate timely billing and collections, ultimately improving financial performance and operational efficiency in healthcare organizations.
How can a team monitor revenue cycle management improvements?
Monitoring revenue cycle management improvements involves tracking key performance indicators (KPIs) such as claim denial rates, payment turnaround times, and accounts receivable aging. Regular analysis of these metrics helps teams identify areas for enhancement and gauge the effectiveness of implemented strategies.
How does a revenue cycle management team work?
A revenue cycle management team works by overseeing the financial process of healthcare services from patient registration to final payment. They ensure accurate billing, manage claims submissions, and handle denials to optimize revenue collection.
How can an organization improve its revenue cycle management?
Improving an organization's revenue cycle management involves optimizing billing processes, enhancing patient engagement, regularly reviewing key performance indicators, and leveraging technology to streamline workflows and reduce claim denials.
What challenges do companies face in revenue cycle management?
The challenges companies face in revenue cycle management include managing billing errors, ensuring timely claims submissions, handling denials effectively, and maintaining compliance with regulatory changes while optimizing cash flow and patient collections.
How can technology enhance revenue cycle processes?
Technology can enhance revenue cycle processes by streamlining workflows, automating tasks, and improving data accuracy, leading to faster claim submissions and reduced denials, ultimately increasing overall revenue for healthcare providers.
What metrics assess revenue cycle management effectiveness?
Metrics that assess revenue cycle management effectiveness include days in accounts receivable, claim denial rates, net collection rates, and clean claim rates, which collectively help gauge the efficiency and profitability of billing processes.
How do changes in regulations impact revenue cycles?
Changes in regulations significantly impact revenue cycles by altering billing practices, reimbursement rates, and compliance requirements. As regulations evolve, healthcare providers must adapt to maintain effective cash flow and ensure accurate claims submissions.
What role does patient engagement play in revenue cycles?
Patient engagement plays a crucial role in revenue cycles by enhancing communication, improving patient satisfaction, and ensuring timely payments. When patients are actively involved, they are more likely to understand their bills, adhere to treatment plans, and facilitate a smoother billing process.
How can revenue cycle management reduce operational costs?
Revenue cycle management can significantly reduce operational costs by streamlining billing processes, minimizing claim denials, and improving cash flow efficiency, ultimately leading to decreased administrative expenses and faster reimbursements.
What software tools assist in revenue cycle management?
Software tools that assist in revenue cycle management include practice management systems, billing software, electronic health record (EHR) systems, and claims processing tools, which streamline processes and enhance financial performance for healthcare providers.
How does coding accuracy affect revenue cycles?
Coding accuracy significantly impacts revenue cycles by ensuring that claims are submitted correctly and promptly. This reduces the likelihood of denials and rejections, ultimately leading to faster payments and improved cash flow for healthcare providers.
What training is essential for revenue cycle staff?
Essential training for revenue cycle staff includes proficiency in medical coding, billing practices, financial analysis, compliance regulations, and the use of electronic health record (EHR) systems to ensure accurate claim processing and revenue optimization.
How often should revenue cycle processes be evaluated?
Revenue cycle processes should be evaluated regularly, ideally on a quarterly basis, to ensure efficiency, identify areas for improvement, and adapt to changes in regulations or market conditions.
What are common revenue cycle management inefficiencies?
Common revenue cycle management inefficiencies include delayed claim submissions, high denial rates, inadequate follow-up on unpaid claims, and poor patient communication, all of which can adversely affect cash flow and overall profitability.
How do payment models influence revenue cycle management?
Payment models significantly influence revenue cycle management by determining how and when healthcare providers receive reimbursement. Different models, such as fee-for-service or value-based care, impact billing processes, cash flow, and the overall efficiency of financial operations.
What is the impact of denials on revenue cycles?
The impact of denials on revenue cycles is significant. Denials can lead to delayed payments, increased administrative costs, and lost revenue opportunities, ultimately affecting a healthcare provider's financial health and operational efficiency.
How can organizations enhance compliance in revenue cycles?
Organizations can enhance compliance in revenue cycles by implementing robust policies, regular training for staff on regulatory updates, and utilizing advanced technology for accurate billing practices and audits. These strategies promote adherence to guidelines and minimize errors.
What strategies improve patient payment collection?
Effective strategies to improve patient payment collection include clear communication of payment policies, offering multiple payment options, sending timely reminders, and providing financial counseling to help patients understand their responsibilities.
How can telehealth services affect revenue cycles?
Telehealth services can significantly impact revenue cycles by streamlining patient engagement and decreasing appointment no-shows, ultimately leading to increased billing efficiency and revenue collection. This modern approach allows practices to broaden their reach and improve patient satisfaction.
What are best practices for revenue cycle management?
The best practices for revenue cycle management include maintaining clear communication with patients, regularly reviewing billing processes, ensuring accurate coding and documentation, training staff effectively, and utilizing technology for tracking claims and managing denials.
How does data analytics aid revenue cycle improvement?
Data analytics aids revenue cycle improvement by identifying trends, pinpointing inefficiencies, and streamlining processes. By leveraging data insights, healthcare organizations can enhance billing accuracy, reduce claim denials, and ultimately increase revenue.
What role does patient information play in revenue cycles?
Patient information plays a crucial role in revenue cycles by ensuring accurate billing, reducing claim denials, and facilitating timely reimbursements. Properly collected and maintained patient data streamlines the entire process, promoting efficiency and profitability for healthcare providers.
How can interdepartmental collaboration enhance revenue cycles?
Interdepartmental collaboration enhances revenue cycles by fostering communication and coordination between departments, leading to improved accuracy in billing, faster claim processing, and reduced denials, ultimately maximizing revenue and operational efficiency.
What trends are shaping the future of revenue cycles?
The trends shaping the future of revenue cycles include increased automation, enhanced data analytics, value-based care models, and a focus on patient engagement to improve collections and streamline processes. These developments aim to maximize efficiency and revenue.
How does reimbursement variability affect revenue cycle management?
Reimbursement variability impacts revenue cycle management by creating uncertainty in cash flow, which can hinder budgeting and financial forecasting. Consistent monitoring and adjustments to billing practices are essential to mitigate these fluctuations and enhance overall revenue.
easycare company, easycare claims, medical billing, medical billing services, medical billing and coding, medical and billing, medical billing jobs, medical billing medical coding, remote medical billing, revenue cycle management, billing coding course medical online, Insurance verification, Denial management, Medical billing companies, Healthcare billing, Medical billing software, Claims processing, Medical billing outsourcing, Medical billing consultant services, Medical billing analyst, Medical billing system software, Eligibility Verification, Medical billing and coding for mental health, Medical billing and coding jobs remote, Medical billing and coding classes near me, Medical billing and coding for chiropractors, Medical billing and coding certification, Medical billing specialist, easycare services, Insurance Pre-Authorization, medical billing services in nj, Medical billing near me, HIPAA-compliant billing, healthcare billing solutions, medical billing specialist, medical billing company, Medical billing software for small business, Best medical billing software for small business, Affordable medical billing software for small business, Medical billing software for startups, Cloud-based medical billing software for small business, Easy-to-use medical billing software, Medical billing software pricing for small business, Top medical billing software for small practices, Medical billing and coding software for small business, Small business healthcare billing solutions, HIPAA-compliant medical billing software, Online medical billing software for small business, Medical billing software comparison for small business, Free medical billing software for small business, Medical billing software features for small business, Medical billing software for solo practitioners, Electronic medical billing software for small clinics, Best cloud medical billing software for small business, Small business-friendly medical billing software, Medical billing automation software for small business., easycare, cardiology medical billing services Pittsburgh, hematology billing services, general surgery medical billing services, ENT medical billing services, orthopedic medical billing services, gastroenterology medical billing services, urology medical billing services, medical billing services Delaware, medical billing companies in Los Angeles, medical billing services in Dallas TX, radiology medical billing services, dermatology billing services, emergency room billing services, dental billing services, mental health billing services, nephrology billing services, ophthalmology billing services, pathology billing services, pediatric medical billing services, podiatry billing services, pulmonology billing services, rheumatology billing services, chiropractic billing services, physical therapy billing services, occupational therapy billing services, speech therapy billing services, anesthesia billing services, pain management billing services, oncology billing services, endocrinology billing services, infectious disease billing services, internal medicine billing services, neurology billing services, obstetrics and gynecology billing services, allergy and immunology billing services, plastic surgery billing services, psychiatry billing services, sports medicine billing services, urgent care billing services, vascular surgery billing services, wound care billing services, medical billing services New York, medical billing services Chicago, medical billing services Houston, medical billing services Phoenix, medical billing services Philadelphia, medical billing services San Antonio, medical billing services San Diego, medical billing services Dallas, medical billing services San Jose, medical billing services Austin, medical billing services Jacksonville, medical billing services Fort Worth, medical billing services Columbus, medical billing services Charlotte, medical billing services San Francisco, medical billing services Indianapolis, medical billing services Seattle, medical billing services Denver, medical billing services Washington DC, medical billing services Boston, medical billing services El Paso, medical billing services Nashville, medical billing services Detroit, medical billing services Oklahoma City, medical billing services Portland, medical billing services Las Vegas, medical billing services Memphis, medical billing services Louisville, medical billing services Baltimore, medical billing services Milwaukee, medical billing services Albuquerque, medical billing services Tucson, medical billing services Fresno, medical billing services Sacramento, medical billing services Kansas City, medical billing services Atlanta, medical billing services Miami, medical billing services Omaha, medical billing services Raleigh, medical billing services Colorado Springs, medical billing services Virginia Beach, medical billing services Long Beach, medical billing services Oakland, medical billing services Minneapolis, medical billing services Tulsa, medical billing services Tampa, medical billing services Arlington, medical billing company in nj, easy care software, medical billing outsourcing, primarycarebillingservicesnewjersey, primarycarebillingservicesnj, easy medical billing